Antibiotic Resistance Inspires Notre Dame to Create New ‘Weapon’
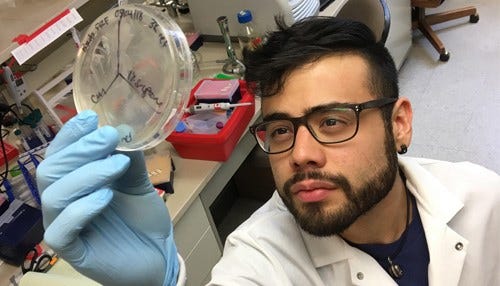 Fields says the lab’s research could lead to a more effective medicine to fight a notorious infection that occurs in burn wounds. (Photo courtesy: Notre Dame)
Fields says the lab’s research could lead to a more effective medicine to fight a notorious infection that occurs in burn wounds. (Photo courtesy: Notre Dame)
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe NowFrancisco "Pancho" Fields knows well the struggle of fighting an antibiotic-resistant infection. Most of his college freshman year was plagued by baths in diluted bleach and multiple rounds of various antibiotics that couldn’t clear a stubborn MRSA infection. The frustration of fighting antibiotic-resistant bacteria sparked Fields’ search for answers, which ultimately led him to a University of Notre Dame lab that aims to unleash a new method of warfare against these elusive infections: using bacteria to fight bacteria.
Antibiotic resistance is considered an increasingly serious threat to public health; the Centers for Disease Control and Prevention (CDC) says more than 23,000 Americans die each year from infections caused by germs resistant to antibiotics. A recent CDC report uncovered more than 200 instances in 2017 of “nightmare” bacteria, which are resistant to most or all antibiotics.
“Most antibiotics target things within the bacteria; resistance usually means the bacteria has changed something within its genetic code, which altered the target of that antibiotic, so now the antibiotic is ineffective,” says Fields, a microbiology PhD student in Notre Dame’s Department of Biological Sciences.
He’s earning respect in science circles for his work in the lab of Shaun Lee, Notre Dame’s Monahan Family associate professor of rare and neglected diseases. Fields recently authored a paper published in The Journal of Antibiotics that details his discovery of using “ancient weapons” in a futuristic way.
Fields’ work centers on bacteriocins, the proteins that bacteria naturally make to kill other bacteria. Fields altered the naturally-produced bacteriocins to make them more effective killers of antibiotic-resistant bacteria. While antibiotics focus on a specific target within bacteria—targets that change, leading to resistance—Fields’ method unleashes a broader strategy.
“[Our proteins] don’t target something very specific; they target the envelope that encases the bacteria. They come into contact with the bacterial surface and kind of just poke holes indiscriminately; and this is what causes the cell death,” says Fields. “Our little proteins have a positive charge, and bacteria tend to have a negative charge, so it’s like a magnet; they attract each other. Once enough of this protein gets on the surface of bacteria, it causes these little holes to form, and that’s what kills the bacteria.”
For the paper, Fields’ research used harmless bacteria commonly found in plants to create the bacteria-fighting proteins. Fields says the proteins showed they could affect both plant and human pathogens, opening the door for many applications.
Burn wounds, for example, can become infected by the antibiotic-resistant Pseudomonas bacteria, which can limit recovery or even be deadly. Fields believes the lab’s research could lead to a topical medicine using natural bacteriocins to more effectively fight the notorious infection.
Fields says the method could also be used in agriculture to prevent bacterial infections in plants and crops.
“Bacteria that affect plants can cause a ton of damage; it’s very, very expensive,” says Fields. “For example, fire blight will kill apple trees and cause damage to orchards, putting farmers out a lot of money. We can see where we could apply these proteins to a plant of interest to protect it from infection.”
A patent is pending on the proteins Fields has developed. The lab is working with Notre Dame’s IDEA Center, which focuses on entrepreneurialism and commercialization, to connect with larger companies that may be interested in licensing the proteins.
While Fields jokes that he “smelled like bleach” while battling his MRSA infection in college, he also acknowledges the seriousness of antibiotic-resistant infections: “[MRSA] could’ve killed me if I just let it get worse.” The infection altered his course, leading him away from medical school and down a more strategic path: finding a new way to kill the most elusive infections.
Fields says his method reprograms bacteria to fight antibiotic-resistant infections.
Fields says the lab’s expertise in skin infections could test the proteins’ ability to kill bacteria in “a more biologically-relevant system.”

