IUPUI Research Could Change Treatment for Some TBIs
 Blazer-Yost says a failed hypothesis during her kidney research uncovered the potential treatment for hydrocephalus.
Blazer-Yost says a failed hypothesis during her kidney research uncovered the potential treatment for hydrocephalus.
Subscriber Benefit
As a subscriber you can listen to articles at work, in the car, or while you work out. Subscribe NowThe Department of Defense has tapped a team of researchers at IUPUI to lead a mission that is critical to the health of U.S. troops. The scientists are working to create a drug to treat hydrocephalus, a condition that often occurs after traumatic brain injury (TBI), which is an increased area of focus for the military due to its high rate of TBIs. The only current treatment for hydrocephalus is brain surgery—an unlikely option during deployment—so the DoD awarded the researchers a nearly $2 million grant to lead the charge for a different battle plan.
The military’s Defense and Veterans Brain Injury Center says more than 375,000 service members have suffered a TBI since 2000; the last few years have posted annual averages that hover around 20,000 TBIs, and the vast majority of those occur during active duty.
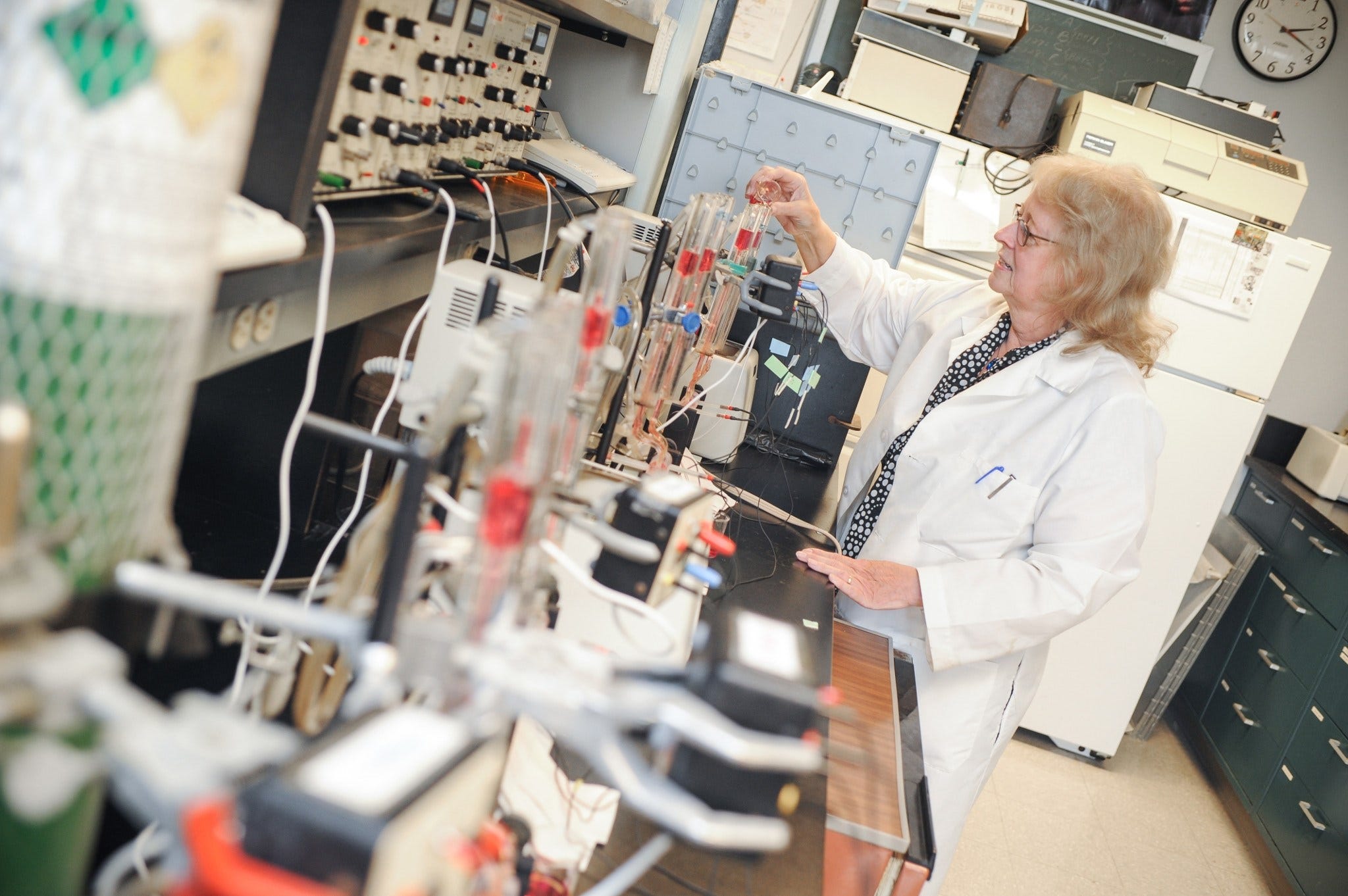
Hydrocephalus, often called “water on the brain,” is caused by cerebrospinal fluid buildup in the skull that makes the brain swell, which can lead to brain damage. IUPUI School of Science Biology Professor Dr. Bonnie Blazer-Yost says data suggests anywhere from 10 to 50 percent of people who sustain a TBI develop post-traumatic hydrocephalus due to inflammation in the brain.
“I think the reason we don’t have good data is, to determine that [you have hydrocephalus], you have to do MRIs, which are expensive and require being near a major medical facility that has that type of equipment,” says Blazer-Yost, the grant’s principal investigator. “So we really don’t know the prevalence of post-traumatic hydrocephalus, but we know it’s a problem.”
The standard treatment for hydrocephalus is brain surgery to insert a shunt that directs the excess fluid elsewhere in the body—a procedure that can be difficult to execute in active military zones. Children born prematurely may also develop hydrocephalus due to brain bleeds. Blazer-Yost says, in these long-term cases, children may undergo many surgeries, because the shunts have a 50 percent failure rate after three years.
The research team has discovered a promising compound that could be an alternative to surgery. It blocks a particular electrolyte channel that’s important for the production of cerebrospinal fluid; in her lab, inhibiting a particular electrolyte transporter reduces hydrocephalus in an animal model.
Blazer-Yost says she stumbled upon the discovery. For many years, her primary focus has been polycystic kidney disease; the compound she’d developed to treat that disease failed, and instead, she uncovered a different application for hydrocephalus.
“Sometimes, a failed hypothesis is a lot more interesting than proving your hypothesis. And in this case, it was, indeed, a failed hypothesis,” laughs Blazer-Yost. “Those of us who have been in science for 30-odd years—you get used to this. I always tell my students, particularly my grad students, don’t become too attached to your hypotheses, because they could be wrong.”
The $1.8 million DoD grant will enable the team, which has been collaborating for several years, to perform more costly and elaborate experiments to further test its compound that could potentially lead to the first non-surgical treatment for hydrocephalus.
In addition to TBI patients and premature infants, such a drug could also help the aging population. Blazer-Yost says one of the most under-diagnosed forms of hydrocephalus occurs in this segment of patients, because it mimics other signs of aging, such as difficulty walking, incognance and dementia.
“There’s a decent incidence of hydrocephalus in Parkinson’s disease, and there are some questions as to whether it might also occur in Alzheimer’s disease,” says Blazer-Yost. “It’s part of a number of different diseases, and I think it’s been more recently recognized.”
Blazer-Yost says the military, especially, is interested in helping soldiers fully recover from TBIs. She acknowledges “it’s a very long way” from the lab to a final drug, but says her team is mission-minded and steadily marching toward that goal.
Blazer-Yost says the military is interested in any treatment that could help service members fully heal from TBIs.
Blazer-Yost says the ultimate goal is to develop a drug to treat hydrocephalus that could be used “as needed.”
